AED Program Best Practices Guide
A Practical Framework for the Placement, Retrieval and Use of AEDs in Workplace and Community Settings
Use of this Guide
Developed and published by:
Readiness Systems
The nation’s leading AED program compliance expert.
© Readiness Systems, LLC – All rights reserved
This AED Program Best Practices Guide is protected by copyright. You are welcome to share the PDF version freely, as long as it remains unaltered. Use, reference, or reproduction of the Guide’s contents is permitted only as specified, with proper attribution, and with the express written consent of Readiness Systems. Publishing, displaying, reproducing, or creating derivative works based on this Guide without express written consent is not allowed.
For more information about this AED Program Best Practices Guide, please contact:
Readiness Systems, LLC
[email protected]
Notice to the Legal Community
This AED Program Best Practices Guide is intended for informational purposes only. It does not establish a legal standard of care, and failure to follow the recommendations outlined in this Guide does not, by itself, imply that an AED program is inadequate or falls below a reasonable level of conduct.
Why this Guide was Created
Sudden cardiac arrest (SCA) continues to be a major public health challenge — even after decades of effort to improve outcomes. Each year in the United States, nearly 400,000 people experience SCA outside of hospitals. About 120,000 of these cases — roughly 30 percent — occur in workplaces and other public spaces. Fast action with cardiopulmonary resuscitation (CPR) and an automated external defibrillator (AED) can save lives, yet survival rates remain extremely low — around 7 percent — largely because AEDs aren’t widely available and too few people are prepared or willing to help.
Only a handful of laws require AEDs in public places, leading to a nationwide shortage. Encouragingly, some organizations have added AEDs voluntarily. But many others hesitate — often because AED programs seem complicated or because of valid concerns about legal liability.
This AED Program Best Practices Guide (Guide) is here to help. It breaks down AED program setup and operations into clear, manageable steps — a practical “how-to” for AED program leaders. It also addresses legal concerns by promoting a realistic and defensible framework built around common sense and community expectations. Having thoughtful written policies not only improves program performance but also strengthens your legal position if a lawsuit arises.
Another key problem: Most people still believe that only those with formal CPR/AED course completion cards can help during an SCA emergency. That myth limits the number of people willing to act — resulting in lost opportunities to save lives.
This Guide challenges that belief and encourages a broader approach. It provides strategies that allow both trained and untrained bystanders to assist in emergencies. The more people who are empowered to act, the greater the chance of survival for someone experiencing SCA.
Bottom line: This Guide aims to increase AED adoption and enable more people to step in and help. The more organizations that say “yes” to AEDs — and the more people willing and ready to respond — the more lives we can save.
Contact Readiness Systems for Custom-Crafted AED Program Policies
This Guide gives you the tools to develop policies and practices for each part of your AED program. Because every organization is different, it doesn’t include one-size-fits-all policies. Instead, your AED program should be built around your specific needs, resources, and environment.
Need help creating customized policies? Readiness Systems can provide tailored support to fit your program.
About this Guide
This AED Program Best Practices Guide was created to help organizations place and use AEDs in workplaces and public settings. AEDs are medical devices meant to be placed where people can easily access them — and they’re designed so that even untrained or minimally trained bystanders can use them to treat SCA. SCA is a life-threatening condition that is always fatal without quick action. Survival depends on starting CPR right away and using an AED as soon as possible.
AED programs are built to support two critical — but rare — actions: enabling bystanders to begin CPR and getting a working AED to someone experiencing SCA. Responding to these events isn’t a medical challenge — it’s a logistical one. The AED itself diagnoses the heart’s condition and delivers a shock if needed.
A complete AED program includes written policies and practical steps that prepare your organization for SCA emergencies, outline how people should respond, and reduce legal risks tied to AED ownership. Industry standards and AED laws help guide what should go into your program.
Understanding Industry Standards and AED Laws
Industry standards reflect common-sense expectations about how AED programs should be designed and run. When organizations create and follow practical, well-thought-out policies tailored to their specific needs, they:
- Meet accepted industry expectations
- Are better prepared to respond to SCA emergencies
- Reduce the risk of poor outcomes
- Strengthen their legal defense if ever sued
AED laws, on the other hand, differ from state to state but typically do one or more of the following:
- Set rules for how AED programs should be operated
- Outline legal protections (often called Good Samaritan immunity) for those involved in AED programs
- Require certain types of organizations to have AEDs
Following AED laws can help preserve legal protections and support your defense if a lawsuit happens. But legal compliance alone isn’t enough — organizations also need strong, practical AED programs to ensure they’re truly prepared for emergencies.
Effective AED programs follow both industry standards and applicable laws — while also considering their own unique circumstances, like their environment, available resources, and organizational goals. Unfortunately, many AED programs are run informally or without a clear structure. This kind of ad hoc approach increases the risk of critical gaps that can lead to preventable deaths from sudden cardiac arrest and lawsuits that are difficult to defend.
This Guide is designed to help organizations avoid those risks. It breaks down every key part of an AED program into clear “building blocks” and offers best practices for doing each one the right way.
AED Program Best Practices
The Three P's of a Successful AED Program
Best practices are proven methods that help organizations get better results by following consistent, effective approaches. Applying these practices to your AED program removes guesswork and helps improve outcomes — while reducing risks.
Preparation
Performance
Protection
Managing Expectations
To apply these best practices effectively, it’s important to understand the real-world challenges AED programs face:
Unpredictable Incidence
Location Infrequency
Responder Inexperience
These realities mean AED programs should not be judged by perfect standards. Most are not run by hospitals or staffed with medical professionals. Instead, their success should be measured by how reasonably they prepare for and respond to rare emergencies.
The Bottom Line
AED programs can increase the chances of survival — but they can’t guarantee it. Following best practices helps your organization prepare, perform, and protect itself when it matters most.
AED Program Building Blocks
A strong AED program is built on a series of essential components — or “building blocks.” Together, these elements form a framework of people, equipment, procedures, and policies that help your organization prepare for SCA and guide how to respond when it happens.
This Guide outlines best practices for each building block, focusing on two key areas:
- Industry standards – These reflect common-sense expectations and are the most critical to program success.
- AED laws – These vary by state and provide important legal requirements and protections.
Below are the core building blocks this Guide covers:
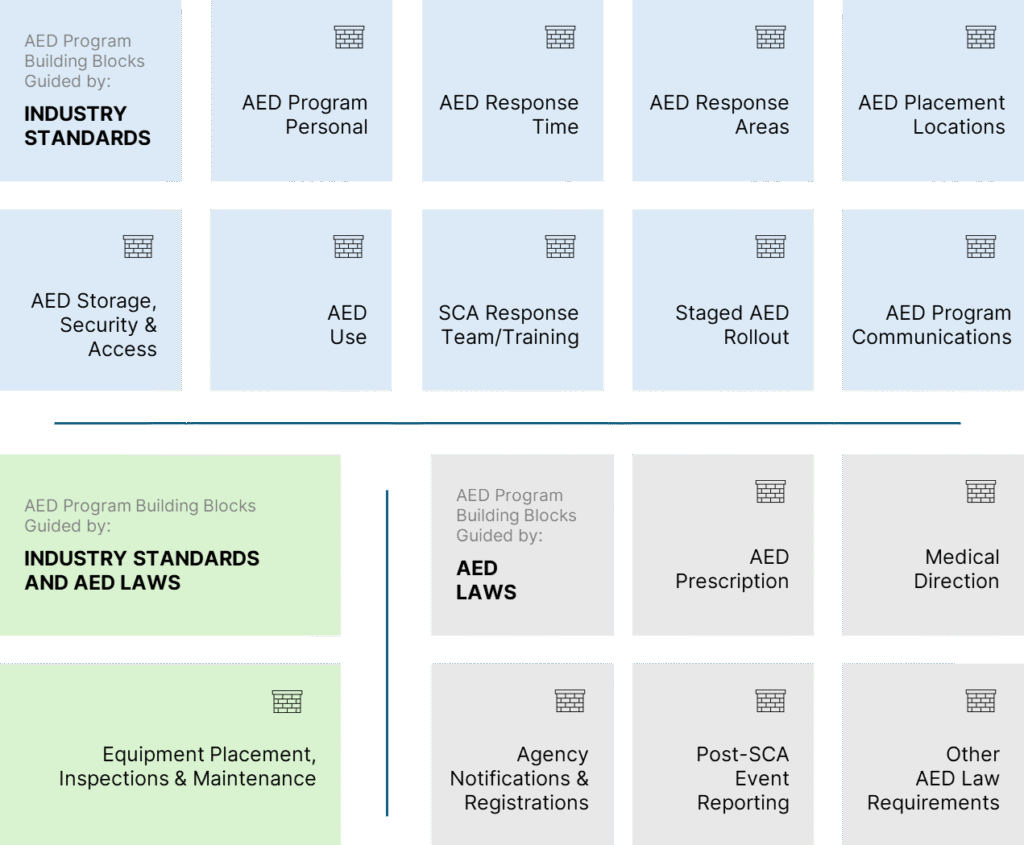
AED Program Building Blocks At-a-Glance
Each part of a successful AED program has its own set of needs. These are shaped by your organization, written into policies, and carried out through day-to-day practices. The list below gives a big-picture view of what’s involved — together, these elements form the foundation of a complete AED program.
- AED Program Personnel: Identify the people involved in your program, define their roles, and assign responsibilities.
- AED Response Time: Set a realistic goal for how quickly an AED should be used after a cardiac emergency is recognized in each area.
- AED Response Areas: Define the specific areas your program will cover, ensuring each can be reached by an AED within your target response time.
- AED Placement Locations: Choose the best locations within each response area to place your AEDs, based on accessibility and response goals.
- AED Storage, Security and Access: Create policies that ensure AEDs are easy to access in an emergency but also protected from tampering or theft.
- Staged AED Rollout: If you can’t install all AEDs at once, plan and document a step-by-step rollout over time.
- Equipment Placement, Inspection and Maintenance: Place all necessary equipment at each AED location and set up a routine inspection and maintenance schedule.
- AED Use: Develop an AED use policy that encourages anyone willing — trained or untrained — to act in an emergency.
- SCA Response Team: Create a response team that includes both trained and untrained volunteers ready to provide CPR and use AEDs.
- AED Program Communications: Share information widely about your AED program, including where devices are located and how people can help.
- AED Prescription: Obtain a required prescription to comply with FDA regulations for most AEDs.
- Medical Direction: In states where it’s required, involve a medical director to meet legal obligations.
- Agency Notifications and Registrations: Where required, notify local agencies about AED locations or register your AED program as needed.
- Post-SCA AED Use Reports: In states that require it, report AED use after an emergency.
- Other AED Law Requirements: Research and comply with any other AED laws that apply in the states where you operate.
Each of these building blocks — and their specific requirements — are explained in detail throughout the rest of this Guide. You’ll find helpful background information along with recommended policies and practices for each one. Organizations that take the time to understand and apply these best practices will be better prepared, more effective, and better protected from risk.
AED PROGRAM BUILDING BLOCKS GUIDED BY INDUSTRY STANDARDS
AED Program Personnel
People are at the heart of every successful AED program. Having the right individuals in clearly defined roles — doing the right things — helps ensure your program runs smoothly both now and in the future. Industry standards highlight five key roles to consider:
Program administration
These individuals oversee the program from a high level. They set goals, approve budgets, make key policy decisions, and assign responsibilities to program managers, site leads, and other team members.
Program coordination
These are the people responsible for administering and keeping the program current. Ideally, you will have at least one overall AED program manager and each AED program site should have at least one site manager. These roles can be combined, and one person can certainly be responsible for multiple AED program sites.
Medical direction
In states that require it, a licensed physician must be involved in your AED program. This is a legal compliance role, not a medical necessity. In states without this requirement, a medical director is not needed because AED programs are operational — not clinical — in nature.
SCA response
These are the volunteers — trained or untrained — who are allowed to perform CPR and use an AED during an emergency.
Equipment inspection and maintenance
This group is responsible for checking and maintaining AEDs and related supplies to ensure everything is ready when needed.
Recommended Policy
Create a written policy that clearly defines these roles and outlines who is responsible for each. Be sure expectations are well communicated and adjust assignments as needed — roles may shift over time or be shared among multiple people.
AED Response Time
Setting a clear and realistic AED response time goal is one of the most important — and most misunderstood — parts of an AED program. A documented response time policy helps ensure your program is judged against practical, real-world expectations rather than unrealistic or legally risky assumptions.
What is AED Response Time?
AED response time is the total time from when a suspected sudden cardiac arrest is first recognized to when an AED is used. This includes four elements:
— Recognizing that someone may be in cardiac arrest
— Deciding to retrieve — or asking someone to retrieve — an AED
— Physically retrieving the AED
— Using the AED on the victim
Why Realistic Goals Matter
Many variables affect how quickly bystanders can respond — human behavior, building layout, available resources, and even program design. These real-world factors make it unrealistic to expect a “perfect” response every time.
Some sources claim that AEDs must be used within three minutes, but no law or industry standard actually requires this. In fact, the so-called “three-minute rule” is misleading and can create unnecessary liability risks.
Instead, your AED response time goal should be a reasonable target, not a promise.
Recommended Policy
This Guide recommends setting a 5-minute AED response time goal for each defined response area in your program. Importantly, your written policy should make it clear that this is not a guarantee — just a good-faith goal designed to reflect what’s realistically achievable.
This five-minute target aligns with emergency cardiac care guidelines and recognizes that:
- AED programs rely on non-medical volunteers
- Non-medical volunteer bystanders are under no legal obligation to act
- AEDs are used in unpredictable, real-life situations — not controlled emergency medical environments
Related Planning Areas: Several other building blocks influence AED response time and should be considered when setting your policy:
- AED Response Areas – Where your AED coverage is planned
- AED Placement Locations – Where AEDs are placed
- AED Storage, Security, and Access – How AEDs are stored and who can get to them
- AED Use – Who is allowed or encouraged to use AEDs
- AED Response Team – Who is authorized to perform CPR and retrieve AEDs
AED Response Areas
An AED response area is a specific part of your site that one AED can reasonably cover within your set response time goal. To determine how large each area can be, you’ll need to factor in things like walking speed, obstacles, and how quickly someone can get an AED and return to the victim.
Time matters in sudden cardiac arrest. The faster an AED is used, the greater the chance of survival. That’s why each AED can only serve a limited area.
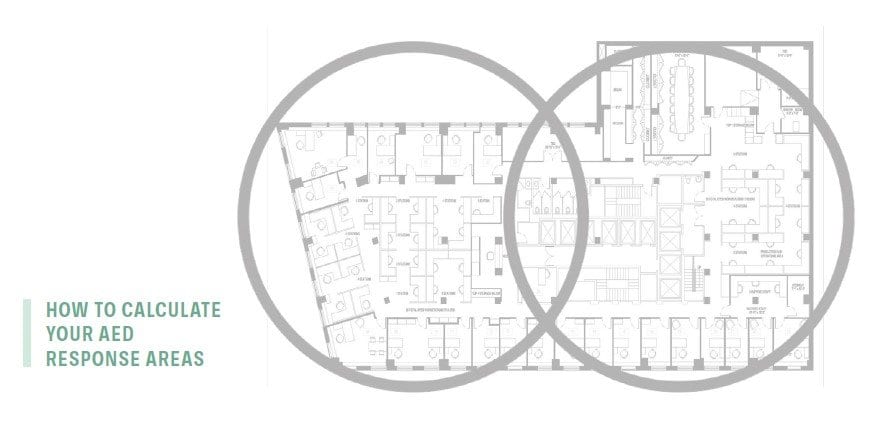
Estimating Your AED Coverage
As a rule, most AED programs allocate 2 minutes of the total 5-minute response time for retrieving the device. Since most adults can walk about 300 feet per minute, a 300-foot radius gives you a rough estimate of the maximum coverage area — about 283,000 square feet (roughly five football fields).
However, real-world obstacles like hallways, doors, stairs, elevators, and crowds can slow things down. If these reduce your walking distance to 150 feet in one minute, your AED’s effective coverage drops to around 70,650 square feet — about 2.5 football fields.
Use this approach to map out how many AED response areas you’ll need to fully cover your facilities. In smaller sites, one AED might cover the entire location. In larger or more complex environments, you’ll likely need multiple AED response areas.
If your program supports public access AED use, consider allowing your devices to be used by neighboring businesses or tenants. This can expand coverage, but it requires coordination, clear policies, and thoughtful risk management.
Excluding Areas from Coverage
There may be valid reasons to exclude certain areas from your AED response plan. Examples include:
- Low foot traffic or usage
- Very low likelihood of SCA
- High costs or logistical challenges
- Limited funding
- Legal restrictions
- Dangerous or high-risk zones
- Proximity to emergency responders
If you choose to exclude areas, be sure to document your reasons — especially if you’re rolling out AEDs over time.
Recommended Policy
This Guide recommends that you create a written policy that clearly defines your AED response areas and explains any exclusions. This helps ensure transparency, supports legal defensibility, and provides a solid foundation for program planning.
Related planning areas:
AED Placement Locations – Where you put the AEDs to support coverage goals.
AED Placement Locations
Once you’ve defined your AED response areas, the next step is to identify specific AED placement locations within each area. Proper placement is critical to ensure rapid access and effective response during a sudden cardiac arrest emergency.
Factors to Consider When Selecting AED Placement Locations
When determining exact AED locations, consider the following:
- Visibility and Accessibility: AEDs should be clearly visible and easy to access by responders.
- High-Traffic Areas: Prioritize locations near entryways, stairwells, elevators, break rooms, kitchens, meeting areas, and other high-use spaces.
- Proximity to Responders: Place AEDs near designated response team members or frequently staffed areas.
- Population Density: Focus on areas where people congregate or work closely together.
- Response Time: Ensure AEDs are positioned to meet your response time goals.
Once placement locations are identified, install an AED and associated supplies at each location.
For guidance on storing, securing, and accessing AEDs, refer to the AED Storage, Security and Access section.
Recommended Policy
Organizations should develop and maintain a written policy that formally designates and documents the AED placement locations across all AED response areas.
Related planning areas:
- AED Storage, Security and Access: Defines how AEDs are stored and who is authorized to access them.
- AED Use: Identifies who is permitted to retrieve and operate AEDs.
- Equipment Placement, Inspection, and Maintenance: Details what equipment is placed at each location and how it is maintained for readiness.
AED Storage, Security & Access
The ability to quickly retrieve and use an AED during a cardiac emergency depends heavily on how the device is stored and secured. While AEDs must be easily accessible, they also need to be protected against theft, tampering, and damage. Balancing accessibility with security is essential to ensuring AED readiness.
Key Considerations
- Accessibility: AEDs must be stored in a manner that allows for immediate and unobstructed access in an emergency.
- Security: Devices should be protected against misuse, theft, or environmental damage without impeding retrieval by responders.
Recommended Policy
This Guide recommends implementing written policies and operational practices that ensure AEDs are:
- Easily accessible when SCA occurs.
- Reasonably protected from theft, tampering, or misuse.
AED Storage and Security Options
Examples of effective AED storage and security practices include:
- Supervised Placement: Locate AEDs in areas where personnel are present or able to visually monitor the device during most operating hours.
- Audible Alarm Cabinets: Use unlocked storage cabinets that emit a loud audible alarm when opened, alerting nearby individuals.
- Real-Time Alert Cabinets: Use cabinets equipped with sensors that detect when the door is opened and immediately send alerts.
- Restricted Access Environments: Store AEDs in secured or unsecured areas that are accessible only to individuals trained and authorized to retrieve them quickly when needed.
- Video Surveillance: Monitor AED storage areas with live video surveillance for added security.
AED Access Policy
This Guide encourages the adoption of policies that allow any willing person to access and retrieve an AED during an emergency. If you choose to limit access:
- Clearly define in writing who is restricted from accessing the AED.
- Document the specific rationale for those restrictions.
Staged AED Rollout
Some organizations may not have the immediate resources to fully implement their desired AED program. In these cases, a staged rollout strategy is a practical and reasonable approach. This allows for the gradual procurement and placement of AEDs over time, aligned with available funding, staffing, and operational feasibility.
While phased deployment may temporarily leave some AED response areas without full coverage, it is often preferable to deploy some AEDs thoughtfully rather than delay the program entirely. However, this strategy requires careful planning, documentation, and execution to minimize legal and operational risks.
Recommended Policy
If your organization adopts a staged AED deployment approach, this Guide recommends creating a written staged rollout policy that addresses the following:
Deployment Planning Considerations
Prioritize AED placement during staged rollout based on:
- Population Characteristics: Number of people and risk factors present in each AED response area.
- Activity Type: Nature of activities (e.g., strenuous, isolated, high-traffic) in each area.
- Response Time Gaps: How AED coverage in one area affects response times in adjacent areas.
- Proximity to EMS: How close each site is to local emergency medical services.
- Site Infrastructure: Availability of facilities and staffing to support AED operation and maintenance.
Required Policy Components
Your written staged rollout plan should include:
- Total Targeted AED Count: The overall number of AEDs to be deployed program-wide and at each program site.
- AED Placement Locations: The specific locations designated for each AED, even if deployment is delayed.
- Initial Deployment Count: Number of AEDs to be placed at program inception.
- Staged Deployment Count: Number of AEDs to be acquired and placed after inception.
- Deployment Timeline: Estimated dates for both initial and subsequent AED placements at specified locations.
Risk Management Considerations
Because SCA events are unpredictable, your staged rollout policy must be based on reasonable judgment and thoughtful prioritization.
To reduce liability risk and ensure accountability:
- Document all placement decisions and deployment timelines.
- Follow through with deployments as scheduled.
A well-documented phased deployment is a recognized and responsible way to build out your AED program in stages, rather than doing nothing at all.
Equipment Placement, Inspection & Maintenance
AEDs are sophisticated electronic medical devices that use internal hardware and software to analyze heart rhythms and deliver a shock (defibrillation) when appropriate. To ensure they function properly in a sudden cardiac arrest emergency, AEDs perform regular self-checks and display visual indicators that show their current readiness status. In addition, AED batteries and electrode pads must be replaced before their manufacturer-specified expiration dates.
While AEDs are rarely used, they must work reliably every time they are needed. Failure to properly inspect and maintain AEDs can result in tragic outcomes — including preventable deaths — and expose organizations to serious legal liability.
Legal and Operational Responsibilities
From both industry standards and AED law compliance perspectives, your organization is responsible for:
- Ensuring AEDs are properly placed and easily accessible.
- Performing routine inspections to verify readiness.
- Conducting timely maintenance, including battery and pad replacements before expiration.
Meeting these obligations reduces the risk of AED failure, supports compliance with applicable laws, and demonstrates a commitment to public safety and risk management.
Recommended Policy
This Guide recommends that your organization adopt a formal policy that addresses the following:
Equipment Placement
- Identify and document the AEDs and related supplies (e.g., accessories, rescue kits) required at each AED placement location.
- Ensure placement complies with the AED response area coverage strategy described in your program plan.
Inspection Procedures
- Define who is responsible for AED inspections.
- Establish a routine inspection schedule. Include checks of AED visual readiness indicators and pad and battery expiration dates.
Maintenance Procedures
- Follow the manufacturer’s user guide for each AED model in use.
- Track, document and complete:
- Battery and pad replacements before expiration
- Repairs or replacements due to damage, failed self-tests, or failed visual checks
Inspection and Maintenance Considerations
AEDs are sophisticated medical devices designed to deliver life-saving defibrillation therapy during sudden cardiac arrest. For an AED to function properly in an emergency, three critical components must be in working condition: the device’s hardware, a charged battery within its useful life, and sealed, unexpired electrode pads that are intact and ready for use.
Ensuring these components are always operational requires a consistent program of inspection, maintenance, and timely replacement. This Guide recommends that organizations assign these responsibilities to specific individuals who are familiar with the equipment and understand the organization’s inspection and maintenance policies.
From a risk management perspective, it’s important that the inspection program includes a structured process to initiate, track, document, and report all inspection and maintenance activity. This not only supports legal and regulatory compliance but also helps prevent failures that could result in avoidable loss of life or liability exposure.
Inspections can be carried out manually by trained staff or through remote AED monitoring systems. Remote monitoring, where available, generally provides more reliable oversight and status updates. Regardless of the method, visual readiness indicators on each AED should be checked at scheduled intervals, and maintenance should be performed both routinely and after any use of the device.
To ensure reliability and accurate recordkeeping, computer-based tracking and reminder systems are strongly recommended. These systems are more dependable than traditional paper logs or spreadsheets and offer better documentation in the event of audits, inspections, or legal scrutiny.
By establishing and maintaining a thorough inspection and maintenance program, your organization can ensure AED readiness, reduce risk, and uphold a critical life safety standard.
A Note About Manufacturer Guidelines
Each AED make and model comes with a manufacturer-provided user guide outlining basic instructions for operation, inspection, and maintenance. As part of your AED program, it is important to review and consider these recommendations when developing your own inspection and maintenance policies.
However, it’s important to understand the limitations of manufacturer guidance. These materials often vary significantly between device models, tend to include general rather than detailed content, and do not offer the level of specificity or comprehensiveness found in an inspection and maintenance program grounded in industry standards.
While manufacturer guidelines are a useful supplement, they should not be relied upon as the sole foundation of your program. Instead, they should be integrated into a broader, more rigorous inspection and maintenance framework designed to ensure AED readiness, reduce risk, and support compliance with legal and professional standards.
A Note About AED Law Compliance
In most U.S. states, AED laws explicitly require AED owners to conduct regular inspections and perform ongoing maintenance. However, regardless of whether a state’s law mandates it, industry standards impose this obligation universally — and courts often look to these standards when evaluating AED program adequacy.
Failure to comply with inspection and maintenance requirements can carry serious consequences. In some states, it may result in the loss of Good Samaritan legal protection, exposing organizations to increased liability. In all jurisdictions, noncompliance can make it significantly more difficult to defend against lawsuits involving an AED’s failure or lack of readiness.
Implementing well-designed, thoroughly documented, and consistently executed inspection and maintenance practices not only demonstrates legal and regulatory compliance but also minimizes the risks associated with AED program failures. A sound compliance framework serves as both a legal safeguard and a public safety imperative.
AED Use
Policies that govern who is allowed to use AEDs — distinct from AED access policies covered in the AED Storage, Security and Access section — directly influence how quickly and effectively these devices are used during SCA emergencies.
A common misconception is that only individuals with formal CPR/AED training and a current course completion card are permitted to use AEDs. In reality, both industry standards and AED laws allow anyone to use an AED. There are no legal or standards-based restrictions prohibiting AED use by untrained individuals.
This means your organization is free to develop AED use policies that leverage all available human resources, thereby maximizing the likelihood of a successful response.
Policy Options
AED use policies typically fall along a continuum:
- Restrictive: Only formally trained individuals may use AEDs.
- Broad: Any willing volunteer may use AEDs, regardless of training status.
- Hybrid: A mix of trained personnel and untrained volunteers are permitted to use AEDs.
Recommended Policy
This Guide recommends adopting a broad AED use policy that allows — and encourages — any willing bystander to use an AED when needed. Empowering all individuals to act increases the chances of saving a life during an SCA emergency.
To support this approach:
- Communicate clearly that everyone is permitted and encouraged to use AEDs.
- Align related policies, including:
- AED Response Team protocols (who may access, retrieve, and use AEDs).
- AED Program Communications (how you inform people of their permission and encouragement to act).
A Note About Volunteer Bystanders
An AED use policy should not be interpreted as creating a legal obligation for any individual — trained or untrained — to act during an emergency. AED use remains voluntary, and individuals must choose whether or not to respond. While no one can be required to help, this policy framework aims to support those who are willing feel empowered to act.
SCA Response Team
An SCA response team consists of one or more individuals who are empowered to perform CPR and access, retrieve, and use AEDs. The composition and size of your team directly influence whether—and how quickly—life-saving action is taken during an SCA event.
This matters because only about 1 in 4 SCA victims receive bystander CPR, and fewer than 4 in 100 receive AED treatment from a bystander. While many factors contribute to these low rates, one major and controllable factor is how AED programs define and manage their response teams.
Here are Some Things to Consider when Developing your SCA Response Team Policies and Practices
Core Concepts
- Team membership is set by your organization’s policies. Your internal decisions determine who is permitted and encouraged to respond.
- SCA response teams are dynamic. Team membership can shift based on staff availability, site operations, and the presence of non-employee bystanders who may be willing to help.
- Anyone can respond. Both trained and untrained individuals can be authorized to perform CPR and use AEDs. Neither industry standards nor AED laws restrict these life-saving actions to trained personnel only.
Differentiating Training and Use Policies
- Training policies define who receives formal CPR/AED training.
- Use policies define who is permitted to act during an SCA emergency — regardless of training status.
- An effective SCA response team includes both trained and untrained individuals who are willing to help.
What AED Laws Say About Training
Many AED laws state that programs must ensure “expected AED users” receive training. However:
- Most laws don’t define who an “expected AED user” is.
- Most laws don’t limit what qualifies as “training.” Accepted formats may include:
- Online-only courses
- Blended online/in-person instruction
- Augmented reality (AR) tools
- Videos, kiosks, or social media platforms
- Traditional classroom learning
This flexibility gives your organization wide latitude to develop a cost-effective, broad approach that still meets regulatory expectations.
Recommended Policy
This Guide recommends implementing a tiered SCA response team policy that defines two categories of responders:
- Category 1 SCA Responders: Individuals with current, formal CPR/AED training who voluntarily choose to respond to suspected SCA events as Good Samaritans. They are encouraged and authorized to perform CPR and access, retrieve, and use AEDs.
- Category 2 SCA Responders: Individuals who do not have current formal CPR/AED training but who:
- Understand the importance of CPR and AEDs,
- Know where AEDs are located,
- Know how to recognize SCA, respond, and use an AED, and
- Voluntarily choose to act as Good Samaritans.
This broad, dual-category framework enables your organization to meet both industry standards and AED response time goals, while maximizing the chances of a successful emergency response.
RECOMMENDED POLICY LANGUAGE
- Category 1 SCA Responders are encouraged to respond to SCA emergencies if available and are authorized to do CPR and access, retrieve, and use AEDs.
- If no Category 1 responder is immediately available or willing to act, any willing Category 2 SCA Responder is authorized to do CPR and access, retrieve, and use AEDs.
This policy gives your organization the best chance that someone will respond when an SCA emergency occurs.
IMPLEMENTATION PRACTICES
To bring this tiered policy to life, this Guide recommends two key actions:
- Formally train a core group of “expected AED users” and make good faith efforts to have at least one formally trained Category 1 responder available in each AED response area during normal business hours.
- Communicate clearly that everyone — trained or untrained — is encouraged and permitted to do CPR and use an AED if they encounter someone experiencing SCA.
FINAL NOTE
AED laws can create the impression that only formally trained people are allowed to respond, but this is not a legal requirement. SCA is unpredictable, and it is unrealistic to expect trained responders to be present at all times. The goal of your policies should be to empower anyone who is willing to act — because someone trying is better than no one acting at all.
AED Program Communications
Internal communications are a key component of an effective AED program. These tools help educate individuals inside and outside your organization — including employees and visitors — about your AED program and prepare them to respond quickly and confidently during an SCA emergency.
By reinforcing awareness and readiness, internal communications support your overall AED response objectives.
KEY COMMUNICATIONS OBJECTIVES
Internal AED program communications should provide:
- Awareness of the AED program’s existence and life-saving value
- Guidance on how to recognize and respond to a suspected SCA emergency
- Visibility through clear signage identifying AED locations
- Engagement via ongoing reminders and updates about the AED program
Recommended Policy
This Guide recommends that your organization periodically develop, distribute, or make available communications that reflect and reinforce your AED program policies. These communications should be designed to inform, empower, and prepare all potential responders.
Recommended content includes:
General AED Program Information
- The purpose and capabilities of AEDs
- The existence and benefits of your AED program
- The locations of AEDs throughout the site
- How to recognize the signs of sudden cardiac arrest
- What to do during a suspected SCA emergency
- How to initiate CPR and retrieve and use an AED
Training Information
- Details about formal CPR/AED training opportunities for employees and other interested individuals
AED Location Signage
Signage plays a vital role in promoting awareness and ensuring compliance with signage requirements found in a small number of states. The following signage practices are recommended:
- At entrances: Post clearly visible signs at commonly used entrances indicating that AEDs are available onsite
- Near each AED: Post signage that clearly identifies the presence and location of the AED and communicates that anyone is permitted to access, retrieve, and use it
AED PROGRAM BUILDING BLOCKS GUIDED BY AED LAWS
AED Prescription
AEDs are classified as medical devices and are regulated by the U.S. Food and Drug Administration (FDA). Although the traditional prescription model does not logically apply in this context — since there is no physician-patient relationship between the AED prescriber and a future SCA victim — the FDA currently requires a prescription for the purchase or sale of most AED models.
This is the only federal-level AED requirement. All other AED-related mandates — including program, maintenance, training, and reporting requirements — are established at the state and local level.
Note
The federal FDA prescription requirement relates only to the sale/purchase of AEDs. This is different from and unrelated to state medical direction requirements covered under Medical Direction.
Recommended Policy
This Guide recommends that your AED program maintain a documented prescription authorizing possession of your AEDs.
You can typically obtain this prescription from one of the following sources:
- Your organization’s medical director (if you have one)
- The AED vendor that sells you the devices
- Your AED program management service provider, if you use one
Keeping a current prescription on file helps ensure compliance with FDA requirements and supports a well-documented AED program.
Medical Direction
So-called AED program medical direction — also known as medical oversight or physician oversight — is a concept created entirely by state-level AED laws. It is sometimes bundled under the broader term AED program management by service providers.
Medical direction requirements were originally included in early AED laws based on the mistaken belief that organizations needed a physician to:
- Direct how SCA should be treated (even though the AED itself provides treatment guidance), or
- Manage the operational logistics of an AED program (which is not a clinical activity).
This premise has never been medically accurate, yet laws in many states still mandate some form of physician involvement.
WHAT THE LAWS SAY – AND DON’T SAY
There is no uniformity in the way these laws are written. Across the states that require medical direction:
- The laws do not consistently define who qualifies as a medical director,
- They do not specify how a medical director should be engaged,
- And they do not clearly outline the scope of tasks or responsibilities.
In real-world practice, the tasks these laws associate with medical direction — such as maintaining documentation or reviewing program procedures — are almost always non-clinical and typically performed by non-physicians.
Bottom line: Having a physician involved in your AED program does not affect your actual emergency preparedness or program performance. It is solely a matter of compliance and risk management.
Recommended Policy
From a compliance perspective, this Guide recommends the following:
- In states that require medical direction:
- Designate a medical director for your AED program. This role can be fulfilled by a qualified internal staff member, or a third-party AED program services provider.
- Ensure there is a documented relationship and scope of work that aligns with the specific requirements outlined in your state’s AED laws.
- In states with no medical direction requirement:
- No medical director is necessary. There is no requirement under industry standards or law to involve a physician.
By structuring your program based on your state’s specific legal requirements, you maintain compliance while avoiding unnecessary administrative burden.
Agency Placement Reporting & Program Registration
Many U.S. states have AED laws that require programs to report AED location information to one or more local public safety agencies. These requirements stem from early AED legislation and — despite their persistence — offer no proven benefit to emergency preparedness or response effectiveness.
These reporting mandates create significant administrative burdens with little to no operational value, for several reasons:
- Ambiguous agency requirements: The laws differ widely and often vaguely reference categories like EMS, 911, fire, or police — but rarely specify which agency must be notified.
- No centralized contact information: With over 3,000 counties and more than 35,000 municipalities and townships in the U.S., determining where to send AED location data — especially across multiple sites — is unrealistic. States do not maintain online directories of required contacts.
- Undefined purpose: These laws do not explain why agencies should receive this information, nor do they require agencies to use or maintain the data in any meaningful way.
- Little to no agency action: With very few exceptions, public safety agencies do not act on AED location data. It is rarely entered into 911 dispatch systems or used to improve emergency response.
In addition to local agency reporting, a few states have state-level AED registration requirements. These mandates can be burdensome and similarly lack demonstrated benefits for AED program readiness or performance.
Recommended Policy
From a legal compliance and risk management perspective, this Guide recommends:
- Make good faith efforts to comply with AED location reporting and registration requirements in states where they exist.
- Document all actions taken, including which agencies you attempted to notify, when and how the notifications were sent, and the content of the communications.
Well-crafted and well-documented agency communications can support your program’s legal defensibility and compliance posture, even if agency response is minimal or nonexistent.
From an industry standards perspective, there is no need to notify any agency or register AEDs in states without such requirements.
Post-SCA Event Notifications
Some states have laws that require AED programs to report incidents where an AED is used. As with other regulatory requirements, these reporting obligations vary significantly across jurisdictions and offer no direct benefits to AED program preparation or performance.
AED use reporting laws present several challenges:
- Inconsistent recipients: eporting targets differ by state and may include:
- State or local agencies
- The AED program’s medical director
- A prescribing physician (often unknown or unrelated to the AED program)
- An unspecified “medical authority”
- Lack of clarity or purpose: These laws do not explain:
- The reason for collecting AED use data
- How recipients should use the information
- What happens after a report is submitted
- No demonstrable benefit: Reporting AED use does not improve response time, device performance, or program readiness. As with medical direction and AED placement notifications, this requirement exists solely for legal compliance purposes.
Recommended Policy
From an AED law compliance and risk management perspective, this Guide recommends:
- Make good faith efforts to fulfill AED use reporting requirements in states where they apply.
- Fully document each step you take, including:
- Who you reported the AED use to
- When the report was submitted
- The contents of the report
Submitting a report — even if the recipient takes no action — can help demonstrate compliance and support your organization’s legal protection goals.
From an industry standards perspective, there is no obligation to report AED use incidents in states that do not have specific legal requirements to do so.
Mandatory AED Placement
In general, organizations are not legally required to have AEDs unless a specific state or local law mandates it. However, a number of states do impose AED placement requirements for certain types of facilities or businesses.
Examples of facility types that may be subject to state-level AED placement mandates include:
- Health clubs and fitness centers
- K–12 schools and colleges
- Dental offices
- Government buildings
- Swimming pools
- Assisted living facilities
- Nursing homes
- Large occupancy buildings
If your organization operates any designated location within a state that mandates AED placement, you are legally required to install and maintain AEDs at those locations.
CONSIDERATIONS FOR NON-MANDATED STATES
If you are required to have AEDs in mandated states, whether you are also legally obligated to install AEDs at locations outside mandated states remains an open legal question. However, from a risk management perspective, a uniform AED deployment strategy — placing AEDs at all locations regardless of state mandates — offers several advantages:
- Greater life-saving potential
- Operational consistency
- Reduced liability exposure
- Simpler program management
If you choose to limit AED deployment only to locations within states that have legal mandates, it is critically important to have documented policies that explain your decision and risk-based rationale.
Recommended Policy
Whether AEDs are installed voluntarily or due to legal mandates, the full set of AED program policies and practices recommended in this Guide should be applied consistently at every location where AEDs are present.
This approach ensures uniform readiness across all sites, compliance with applicable laws, alignment with industry standards, and reduced exposure to legal risk
Other AED Law Requirements
Every U.S. state has laws that govern the ownership and use of public access AEDs — but no two states are exactly alike. While this Guide addresses the most common and widespread requirements, some states impose additional or unique obligations not covered here.
Covering all state-specific variations is beyond the scope of this Guide.
IMPORTANCE OF AED LAW RESEARCH
From an AED law compliance and risk management perspective, it is essential that you:
- Identify and document all legal requirements that apply in each state and jurisdiction where your organization has AEDs.
- Ensure your AED program complies with both general AED laws and any location-specific obligations that may exist.
Recommended Policy
To protect your organization and maintain compliance:
- Research applicable AED laws for every location where AEDs are installed.
- Document all findings and keep them up to date.
- Rely only on reliable, current information, whether you conduct the research internally or use a third-party service.
This due diligence helps ensure reasonable legal compliance and strengthens your organization’s risk management posture.
The Fine Print
This Guide is designed to provide trusted, informed, and comprehensive guidance to help you establish and operate an effective, compliant, and risk-managed AED program. However, because every organization and AED program is unique — and given the litigious nature of the environments in which we operate — it is necessary to include the following disclaimers and limitations.
DISCLAIMER OF LIABILITY
Readiness Systems disclaims any liability for personal injury, property damage, or other harm of any kind — whether direct, indirect, special, consequential, or compensatory — that may result from the publication, use of, or reliance on this Guide.
NOT LEGAL ADVICE
This Guide is provided for informational purposes only. It is not legal advice, does not constitute legal services, and should not be relied upon as a substitute for professional legal counsel. Readiness Systems does not offer or provide legal advice or legal representation.
LIMITED-SERVICE WARRANTIES
- No guarantee of outcomes: Readiness Systems makes no representations or warranties regarding the outcomes of implementing or operating an AED program based on the content of this Guide.
- No professional duty assumed: By publishing and distributing this Guide, Readiness Systems is not undertaking to provide professional services, nor assuming any duty on behalf of any person or entity. Users of this Guide should exercise independent judgment and, where appropriate, seek guidance from qualified professionals.
LAWS AND REGULATIONS
Users are responsible for consulting all applicable federal, state, and local laws and regulations. This Guide is not intended to promote or suggest actions that are inconsistent with applicable law and should not be interpreted as advocating noncompliance.
NOT A STANDARD OF CARE
This Guide does not establish a legal standard of care, nor does deviation from its contents imply that an AED program is inadequate or legally deficient. The recommendations in this Guide are best practice suggestions, not binding standards.